Cancer cases in children and young people up 40% in past 16 years
4,000 children and young people develop cancer every year in the UK, and cancer is the leading cause of death in children aged 1-14 years in the UK.
5th September 2016
4

- 1300 more cancer cases a year* in children and young people (0 – 24 years) compared to 1998 at an extra cost of £130m per year to the NHS.
- Every day in the UK, 10 children and young people are diagnosed with cancer.
- Children with Cancer UK hosts an international scientific conference, showcasing state-of-the-art translational science in childhood cancer – London 5th-7th September.
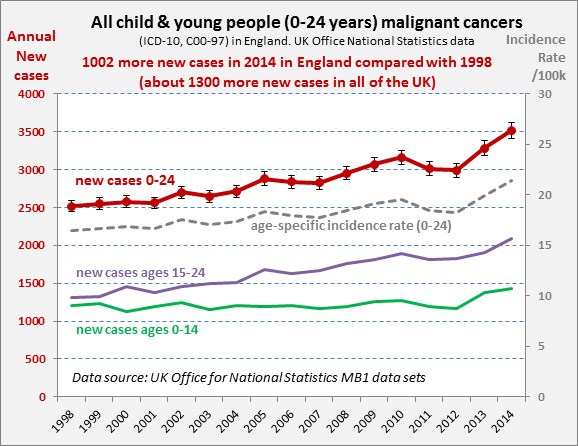
The reasons for this increase are unclear, but the number of children and young people diagnosed with cancer has increased by 40 per cent in the last 16 years, while the incidence rate per 100,000 has risen 30 per cent in the same period (the 10 per cent difference is due to an increase in population). These figures are from a new analysis of official ONS statistics by Children with Cancer UK, the leading national charity dedicated to research into childhood cancer.
To coincide with Childhood Cancer Awareness Month, Children with Cancer UK is hosting Childhood Cancer 2016 (September 5-7), a three-day international conference showcasing state-of-the-art translational science in childhood cancer. Precision medicine is an emerging approach for disease treatment and prevention that takes into account individual variability in genes, environment, and lifestyle for each person.
To transform the lives of every young cancer patient in the UK we need:
- Greater investment in treatment for high-risk cancers with extremely poor survival rates – such as brain tumours, the biggest cancer killer of children.
- Kinder treatments, to reduce the impact that aggressive, toxic cancer treatments have on young patients as they transition to adulthood.
- Better understanding of the causes and prevention of childhood cancer.
The first day of the conference (Monday 5th September) is dedicated to precision medicine treatments which have huge potential in improving cure rates and reducing toxicity in the treatment of children with cancer. Precision medicine involves the use of new treatments to target specific changes in individual patients’ tumour DNA. This is in contrast with existing chemotherapy options that use toxic drugs to kill cells in a much less targeted, less efficient way. Children with Cancer UK calls on government and the science and medical community to ensure that all children diagnosed with cancer in the UK have access to precision medicine by 2020 – launching a 5-point plan on what needs to happen to make this a reality.**
The second day of the conference (Tuesday 6th September) is dedicated to immunotherapy, which is the most promising new cancer treatment since the development of chemotherapy in the 1940s. Whilst it is still relatively early in development, modern immunotherapy offers real hope of curing young patients with the hard-to-treat cancers that have such a poor outlook today, and with a much lower burden of toxicity than the current intensive treatments impose on today’s young patients. Children with Cancer UK is committed to supporting the ongoing development of immunotherapy for children with cancer and is funding a number of important projects at Great Ormond Street Hospital / UCL Institute of Child Health and other centres around the UK.
Dr Nick Goulden, Medical Director at Children with Cancer UK, said:
“There is early evidence that precision medicine works in childhood cancers and can save lives. Crucially for young patients, such targeted therapies could also reduce the burden of toxicity, and help them to improve quality of life both during and after treatment.
However, whilst some colleagues in the US and Europe are already systematically applying this technology to young cancer patients and seeing some success, efforts in the UK have been ad hoc rather than systematically applied in clinical trials.
We need the NHS, pharmaceutical companies and government to prioritise support of the medical and scientific community in their efforts to ensure that all children, teenagers and young adults diagnosed with cancer in the UK have access to precision medicine within the framework of clinical trials by 2020.”
With cancer cases in children and young people up 40 per cent in past 16 years*, the third day of the conference (Wednesday 7th September) considers what we know about influenceable causes of childhood cancer, and the practical measures that might help prevent cancer in children.
The 16-year overall rise is mostly due to teenage and young adults (TYA) 15 – 24 years old. The rises have been most stark in certain cancers, with colon cancer up 200 per cent, thyroid cancer more than doubled (110 per cent), ovarian cancer up 70 per cen and cervical cancer up 50 per cent.
Professor Denis Henshaw, Scientific Director at Children with Cancer UK, said:
“These significant rises in cancer cases cannot be explained by improvements in cancer diagnosis or registration alone – lifestyle and environmental causal factors must be considered.
We need a better understanding of the risk factors for cancer in children and young people, and whether there are practical measures that might reduce exposure to these risks.
If we could prevent 100 cases per year for an investment cost of less than £10m per year, then that would be a net saving for the NHS and taxpayers – and significantly less suffering for the children, young people and their families.”
*All child and young people malignant cancers, 1998-2014
** 5-point plan on what needs to happen to ensure all children diagnosed with cancer in the UK have access to precision medicine by 2020
• To provide somatic and germ line samples within two weeks of diagnosis or relapse.
• Initial funding to be led by charities such as Children with Cancer UK with a commitment from the NHS to fund as service after proof of principle in clinical trials.
• DoH to rapidly establish multi stakeholders’ group to define ethical guidelines for genetic testing in paediatric cancer drawing on international expertise.
• NHS/DoH to develop quality framework for genetic testing including pre and post analytic quality assessment.
• Genetic and clinical data to be stored in a secure digital personal medical record.
• On-going support of a national molecular tumour board of scientist. and oncologist. that makes treatment recommendations based on personal medical record.
• Precision cancer medicine in children to be given a central place in the evolution of UK strategy for analysis of big data in healthcare – so that key data from individual digital personal records can be used anonymously to refine the predictive value of testing for future patients..
• Pharma incentivised to make “targeted drugs” known to have potential activity against a molecular lesion found in a patient’s tumour available for children, and to work harder to provide child-friendly drug formulations.
• Regulators and commissioners to accept, facilitate and fund off-label use of targeted drugs in children if recommended by national / international tumour board.
• Priority given to development, and participation, of the UK in both small proof-of-concept and large scale multinational trials of targeted therapies.
About Childhood Cancer 2016
Childhood Cancer 2016 is an international conference showcasing state-of-the-art translational science in childhood cancer, taking place at Church House Conference Centre, Dean’s Yard, Westminster, London SW1P 3NZ on 5th-7th September 2016.
Combining a line-up of outstanding plenary speakers from the UK, Europe and the US and with free communication and panel debates, we will address three themes over three days:
- Is precision medicine a reality for children with cancer in 2016? Chaired by Professor David Walker and Professor Louis Chesler
- Can we harness the power of the immune system to cure childhood cancer? Chaired by Professor Persis Amrolia and Professor John Anderson
- What do we know about influenceable causes of childhood cancer? Chaired by Professor Denis Henshaw and Professor Tariq Enver
Press enquiries:
For all press enquiries, please email [email protected] or call 0800 222 9000 and ask for the media team.
Other stories
We have lots of information to help you learn more about childhood cancer. From specific cancer types, to treatments and causes.