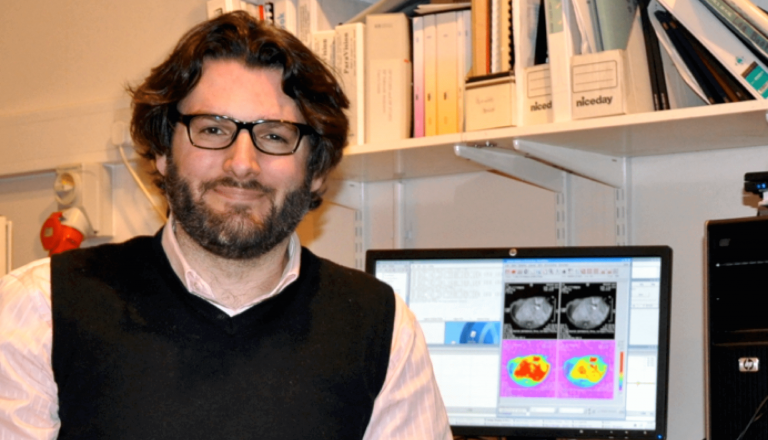
Dr Yann Jamin BSc (Hons), PhD
Children with Cancer UK Research Fellow, The Institute of Cancer Research, London
Dr Yann Jamin is an expert in molecular and functional imaging applied to cancer. Dr Yann Jamin is a junior group leader at the ICR since 2014 and his research focus on Magnetic Resonance Imaging (MRI).
His research used advanced mouse models of neuroblastoma and computer-aided digital pathology to calibrate non-invasive MRI-based functional and molecular imaging scans to reveal and maps regional variations in active disease and to monitor and predict how neuroblastoma respond to therapy. Collaborating with the Royal Marsden Hospital and Great Ormond Street Hospital, he aims to translate these scans into practical solutions to enhance the clinical management of children with neuroblastoma.
His goals are to improve radiological diagnosis and response assessment while both shedding new lights on the biology of the disease and accelerating the development of more effective and safer therapies for children with cancer
In May 2014 he was awarded a Children with Cancer UK Research Fellowship to help him to take forward these ambitions. Dr Yann Jamin joined our Scientific Advisory Panel in April 2016.