Research
Discovery, development, and delivery of effective combination therapies for high-risk medulloblastoma
One of the major specific challenges in childhood cancer is Group 3 medulloblastoma driven by the over-abundance of a gene called MYC (MYC-MBGroup3). This tumour group occurs almost exclusively in young children and is essentially incurable, contributing significantly to overall childhood cancer death rates. New targeted treatments are urgently needed to improve the outlook for children with high-risk medulloblastoma. The INSTINCT-MB project will seek to develop new treatments for MYC-MBGroup3, using new drugs and promising new immunotherapies known as Chimeric Antigen Receptor T-cells (CAR-T) therapies.

Project Details
- INSTINCT-MB: Strategic implementation of novel combination therapeutics for high-risk medulloblastoma
- Lead Researcher
- Professor Steve Clifford
- Research Centre
- Newcastle University Centre for Cancer, Newcastle University
- City & Institution Postcode
- Newcastle upon Tyne, NE1 7RU
- Start Date
- 1 February 2022
- Project Duration
- 60 months
- Grant Amount
- £712,027 co-funded by Blue Skye Thinking and Little Hero
Overview
Brain tumours are the most common tumours that develop in children. Medulloblastoma is the most common malignant brain tumour affecting children. Over the last 50 years, advances in standard treatments such as surgery, radiotherapy and chemotherapy have led to long-term survival rates of approximately 70%. However, survival rates have plateaued, and current therapies are associated with significant long-term side effects in surviving patients. New therapies are urgently required to improve the outlook for children with high-risk medulloblastoma. MYC-MBGroup3 represent one of the major current challenges in paediatric oncology, carrying the worst prognosis of all medulloblastomas, accounting for a high proportion (5-10%) of childhood cancer deaths and is one of the major causes of disease relapse. Yet, the MYC-MBGroup3 disease group shows the most promise for the development of new targeted treatments. The team have developed new immunotherapies for medulloblastoma and shown in initial research that local delivery of CAR-Ts into the fluid surrounding the brain is achievable, and a highly effective approach for their administration.
Project Description
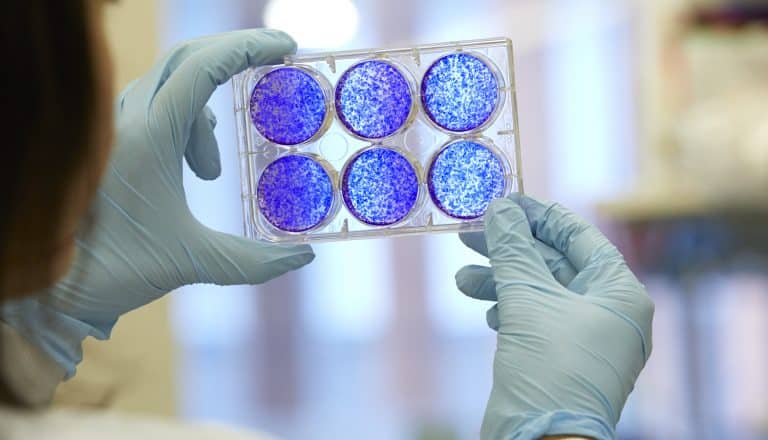
This innovative project, co-funded by Children with Cancer UK, Blue Skye Thinking and Little Hero, aims to develop new treatment regimens for MYC-MBGroup3. To address this challenge, and minimise the chance of treatment-resistance, the team will assess and combine two different treatment approaches: drugs which indirectly-target MYC (MYC targeting), and a type of immune therapy, CAR-T, which is also designed to target MYC-driven medulloblastoma. Professor Steve Clifford and his team have developed a series of experimental models which recapitulate the disease in children as closely as possible. Using these models, they will develop a deep understanding of the biological vulnerabilities of these tumours. Based on these findings, they will further develop and deliver new MYC-targeting drug and CAR-T treatments, test regimens for administration, and generate the essential evidence required to directly translate this work into clinical studies in children with medulloblastoma. Knowledge gained from pre-clinical trials will track how tumours respond to treatment, identifying potential mechanisms of treatment resistance.
Potential impact
The team anticipate the treatment approaches developed by this project will help to reduce the incidence of disease relapse and the late-effects associated with current standard of care treatments for children with relapsed medulloblastoma and treatment-resistant MYC-driven medulloblastomas. The leading roles of Professor Clifford and his team in international pre-clinical and early clinical networks will help to direct the translation of results to human clinical studies.
About the Research Team
Professor Steve Clifford is a Professor of Molecular Paediatric Oncology and Director at the Newcastle University Centre for Cancer. Professor Clifford is a proven organisational lead of international clinical research networks and is working with a team of highly experienced international leaders in medulloblastoma research. The multi-disciplinary team comprises the essential expertise to deliver new therapies from concept to clinic and, importantly, involves emerging independent investigators: Dr Rebecca Hill of Newcastle University, Dr Laura Donovan of UCL and Dr Alejandra Bruna of ICR. They will be working alongside established senior investigators – Professor John Anderson of UCL and Professor Louis Chesler of ICR. Their work will also be supported by international collaborators Professor Gareth Veal, Professor Andrea Sottoriva, and Professor Robert Wechsler-Reya.
Other stories
We have lots of information to help you learn more about childhood cancer. From specific cancer types, to treatments and causes.