The case of Allison Schablein, a young brain tumour patient from the US
This case demonstrates the premise of precision medicine. Allison was four years old when doctors found multiple tumours in her brain and spine. One tumour was removed surgically; the remainder were surgically inaccessible and quickly became resistant to
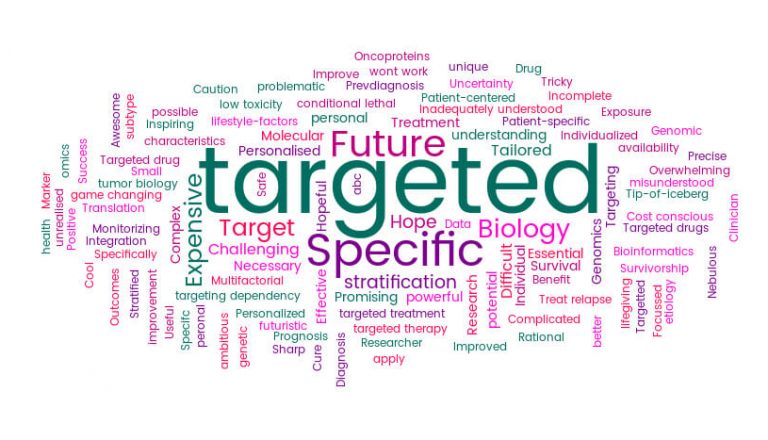
chemotherapy. There seemed to be nothing else that doctors could do for Allison until genomic testing revealed that her tumours had a genetic mutation called BRAF, seen in some cases of the skin cancer melanoma. Allison was enrolled onto a clinical trial of dabrafenib, a drug targeting the BRAF mutation in (adult) melanoma patients.
Within two months, Allison’s tumours were gone or, at least, had shrunk so much they were no longer visible on an MRI scan. Three years on, there are still no visible signs of any tumours. As with the implementation of any new and highly promising approach, we need to fully understand how the genetics of each tumour predicts which patients will respond most effectively, and in which circumstances.Whilst it might seem odd to treat a skin cancer and a brain tumour with the same drug, this demonstrates the difference in the precision medicine approach, where
treatment is based upon common mutations rather than the location of the tumour. The arrival of a new generation of targeted ‘precision’ cancer drugs that attack tumours with specific genetic mutations opens up the possibility of new, more targeted treatments for young cancer patients as well as the possibility of access to drugs designed to treat adult cancers. We hope that by matching the best-targeted drugs to patients using the most precise information about their tumours, we will
maximise the promise and minimise the toxicity of this new generation of drugs. Of course, treatment is not likely to be universally effective. And, as with any new approach, there will be complications of treatment. Some children will fail to respond and others will develop resistance. As with the implementation of any new and highly promising approach, we need to fully understand how the genetics of each tumour predicts which patients will respond most effectively, and in which circumstances.